Is Glucose Reading of 89 in Morning Good?
Abstract
Assay of real-globe glucose and insulin clinical data recorded in electronic medical records tin provide insights into tailored approaches to clinical intendance, nonetheless presents many analytic challenges. This work makes publicly available a dataset that contains the curated entries of blood glucose readings and administered insulin on a per-patient footing during ICU admissions in the Medical Information Mart for Intensive Care (MIMIC-Iii) database version i.4. Besides, the nowadays study details the information curation process used to extract and match glucose values to insulin therapy. The curation process includes the creation of glucose-insulin pairing rules according to clinical proficient-defined physiologic and pharmacologic parameters. Through this arroyo, it was possible to align nearly 76% of insulin events to a preceding claret glucose reading for nearly 9,600 critically ill patients. This work has the potential to reveal trends in real-world practice for the management of blood glucose. This data extraction and processing serve as a framework for future studies of glucose and insulin in the intensive care unit of measurement.
| Measurement(southward) | Claret Glucose • insulin (human) |
| Technology Type(southward) | glucose analyzer • glucometer • Electronic Medical Record |
| Gene Type(s) | glucose readings • insulin inputs |
| Sample Characteristic - Organism | Homo sapiens |
Machine-accessible metadata file describing the reported information: https://doi.org/10.6084/m9.figshare.13564187
Background & Summary
There are relatively few randomized controlled trials that study glycemic control in the intensive care unit (ICU) setting. This is due to the complexity of studying large populations and standardizing protocols for managing glucose across unlike medical centers. Current clinical exercise guidelines are general and recommend avoiding both hypoglycemia and hyperglycemia in critically ill patientsi.
Retrospective assay of real-earth data can potentially reveal valuable insights into specific ranges of glycemic targetsii which may provide a survival advantage for certain populations of critically ill patients. The currently available large real-world data sets are not suitable in their unprocessed course to answer these important clinical questions. Here we present a comprehensive approach to the extraction and processing of insulin treatments and claret glucose readings of critically ill patients from electronic medical records.
The post-obit analysis demonstrates how to convert database queries of unprocessed glucose and insulin values into a clinically validated and reproducible dataset. It highlights the challenges of interpreting the variable of blood glucose level while it is measured in two dissimilar and contemporaneous methods. It proposes how to stratify the multiple unlike types of insulin administered in the ICU. Besides, it shows how to create time-serial records at the individual patient level of measured blood glucose versus the dose of administered insulin. The process of pairing each administration of insulin to a corresponding glucose value allows for the potential cosmos of a model that shows both how glucose is managed in the existent-world and too how patients respond to this therapy in a per-patient time series for each specified ICU admission in the dataset.
The present paper used existent patient blood glucose and administered insulin values to create these individual time series records. Information technology was employed the MIMIC-3 v.1.four databasethree, a publicly available dataset, contains over 58,000 hospital admissions from approximately 38,600 adults. Identifying these patients through traditional manual chart review would exist impractically time intensive. The primary challenges of our project were (1) matching a dose of regular insulin to the specific glucose value that triggered the treatment and (2) identification of values that were likely erroneously entered for both blood glucose entries and insulin entries. The reason erroneous entries exist is that documentation in electronic medical records is subject to human fault and tin can be limited due to other clinical priorities in the ICU. For that purpose, it was necessary to create, interrogate, and iteratively refine rules to pair and marshal each insulin effect to the preceding claret glucose. The rules were derived from a consensus betwixt a group of clinicians, including an internist, an intensivist, and an endocrinologist. The clinicians derived the rules from physiologic and pharmacologic standards.
Data scientists first sorted and identified specific subgroups of patients, equally defined by clinical experts. This then allowed clinical experts to identify erroneous entries of blood glucose and insulin doses. This identification step requires consideration of the type of insulin, timing of administration, timing of glucose measurement, institutional nursing practices, and glucose values. For example, clinicians are not only necessary for defining abnormal values, just also identifying appropriate parameters for linking glucose to insulin administration based on clinical protocols; and identifying scenarios when "outlier" glucose readings may represent true values and non errors. This stride of data curation is crucial before any motorcar learning can exist performed4,5,6.
Figure 1 outlines the experimental workflow used to curate glucose readings and insulin inputs, and posterior merging to create one data subset for future analysis. Access to the complete lawmaking to reproduce this information curation process is provided to let others to continue to generate insights related to the direction of blood glucose in the ICU. Too, the codes of the validation assays for this data subset are provided.
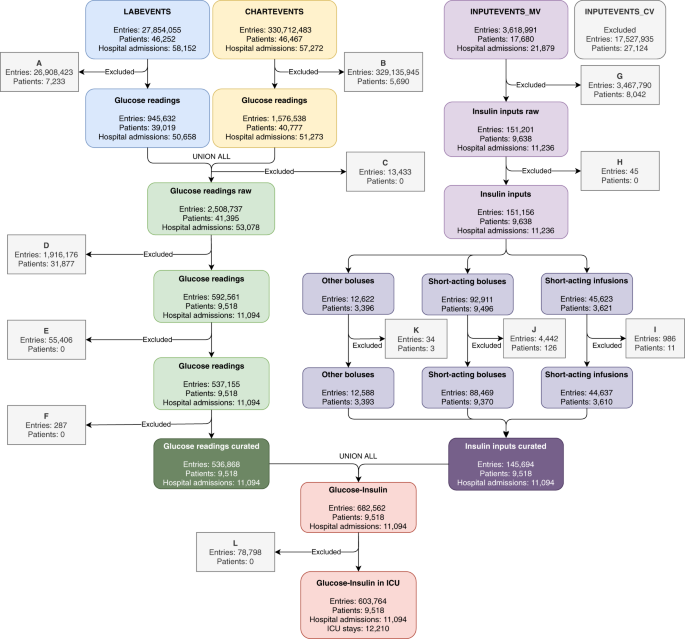
Inclusion criteria for information curation process. Refer to the Methods department to follow and read this figure entirely.
Through sharing this data curation process of paired glucose and insulin values, it is publicly available to provide a reference framework for extracting and matching real-globe hospital data. We provide a detailed methodology to assistance future research around glycemic control in the ICU using existent-world data. Thus, this report tin can also be used as a starting point for retrospective assay of outcomes in the ICU, inform future clinical trial designs, and generate new treatment approachesseven,viii. Also, nosotros highlight that potent collaboration between clinical experts and data scientists must exist from the beginning of these projects to improve the validity of data representation – for example, the pairing of insulin and glucose readings.
Methods
The post-obit subsections describe the extraction and processing of the information required to understand glucose control during an ICU stay. The chief categories of data called for extraction were glucose readings and insulin inputs. All ICU stays with at least i event of glucose reading and/or insulin input were included. It is suggested to read these subsections along with Fig. 1.
Data extraction and Pre-processing
Glucose information drove
In the ICU setting, patient blood glucose values are measured using either laboratory chemical science analyzers or bedside fingerstick glucometersnine. In MIMIC-III, laboratory analyzer glucose values are recorded in the LABEVENTS and CHARTEVENTS tables (Fig. 1). Fingerstick glucometer measurements are simply recorded in CHARTEVENTS. Glucose values were recorded beyond 10 different Detail IDs in MIMIC-III (Table 1), 7 Item IDs within the CHARTEVENTS table, and iii Item IDs within the LABEVENTS tabular array. The raw number of instances of glucose recordings was ii,508,737 within a population of 41,395 patients after merging the Item IDs referred to in Table ane and removing glucose values that were zero or recorded equally an error. These errors occurred during the measurement in the hospital (https://mimic.physionet.org/mimictables/chartevents/). Erroneous entries are indicated in the Fault column from the CHARTEVENTS tabular array as not recorded or recorded as 1 (criteria A and B Fig. i).
And so after joining the information of the LABEVENTS and CHARTEVENTS tables, the remaining null values, where no result was recorded, were removed (benchmark C Fig. one). Posteriorly, patients who did not receive any insulin were excluded (criterion D Fig. 1). Duplicate values were removed when identical readings with the same timestamp and glucose values appeared in both LABEVENTS and CHARTEVENTS (criterion Due east Fig. 1).
To further curate the glucose readings, the following considerations were taken into account:
-
Glucose measured from the laboratory analyzer is considered more accurate than the fingerstick glucometer, especially at higher glucose levels. All the same, in the clinical setting fingerstick glucometer measurements are used oftentimes and insulin can exist dosed based on fingerstick measurements solitary. Therefore, both methods of glucose measurement were included in the extraction scripts.
-
Glucose measurements were extracted with the following rules (benchmark F in Fig. 1):
-
All glucose values ≥grand mg/dL were removed. These values were removed because they were above the limit of accurate measurement for the laboratory analyzer used at Beth Israel Deaconess Medical Center (BIDMC).
-
If a sample was taken from serum and the value was <1000 mg/dL, then that glucose value was included.
-
If a sample was taken with the fingerstick method and the value was <500 mg/dL, then that glucose value was included. It was determined that in this dataset, all fingerstick values above this threshold were simply recorded equally "500". These values were removed because they are above the limit of accurate measurement for the fingerstick glucometer analytical method used at BIDMC.
-
The time stamps recorded for glucose readings are based on charting by nursing staff in the ICU. Due to other clinical priorities and patient intendance issues, in that location may exist errors in the time postage stamp as entered by the nurses. To account for this, the post-obit assumptions were made:
-
Sometimes the STORETIME (fourth dimension listed past nurses for checking glucose) was recorded before the CHARTTIME (the time when the actual information entry occurred). In that case, the STORETIME timestamp was considered to exist the time when the glycemic check occurred. Otherwise, the CHARTTIME timestamp was maintained equally the time of glycemic check (criterion F of Fig. ane).
The inclusion criteria described above resulted in 536,868 instances of unique glucose measurements within a population of 9,518 patients who received insulin during their admission to the hospital. The number of raw and curated instances of glucose measurements for each Detail ID are also displayed in Table one.
The number of entries that accept values above the limit of accurate measurement for each belittling method, were non significant. Only 144 entries for blood samples analyzed in the laboratory were removed (0.06% of entries remaining after applying criterion F in Fig. 1). In the case of bedside fingerstick samples, 146 entries were removed (0.05% of entries remaining later applying criterion F in Fig. 1). Presumed delays in the recording of the glucose readings occurred in 44,926 cases, which represents 8.4% of the total glucose readings (due north = 536,868; criterion F in Fig. 1). The median of this delay was 25 min.
One time all of these criteria were considered, the values were merged with the curated subset containing the insulin inputs (Fig. one). Once beingness merged, the remaining glucose readings occurring outside the ICU stay were removed (criterion Fifty in Fig. 1).
Insulin data collection
In the ICU, insulin is administered every bit a medication to control hyperglycemia. In that location are many forms of insulin and they are classified according to the duration of their effect, curt (iv–viii hours), intermediate (10–12 hours), or long (12–24 hours). Insulin is also classified based on the road of administration including intravenous continuous infusion, intravenous bolus, or subcutaneous bolus. Infusions and boluses in MIMIC-III, including type, are recorded in the INPUTEVENTS_CV (CareVue by Philips) and INPUTEVENTS_MV (MetaVision by iMDSoft) tables (Fig. 1). CareVue covers the menses from 2001–2008, while MetaVision covers the years from 2008–2012.
Since MetaVision provides richer features (e.g.: insulin blazon), just MetaVision records were curated as shown in Fig. one. The events with the flag rewritten and/or related to other inputs were removed (criterion G in Fig. 1). Rewritten entries are wrong inputs that were not delivered to patients (https://mimic.physionet.org/mimictables/inputevents_mv/). Thus, the rates and amounts described were excluded. Insulin assistants events were recorded in vi different detail IDs in MIMIC-III, each respective to a dissimilar type of insulin. The raw number of instances of insulin administration was 151,201 within a population of 9,638 patients.
Insulin administration events that did not take an associated ICU stay ID (i.e.: blanks or aught values) were removed equally well (criterion H in Fig. 1). These events occurred outside of the ICU setting.
It is important to note that insulin infusions and insulin boluses are recorded differently. Infusions are recorded when the infusion is started, when the rate is changed and when the infusion is discontinued. The duration of a certain rate of infusion is used to calculate the amount of continuous infusion of insulin administered within a time window. This is unlike from insulin boluses which are documented as split up events.
For further curation, some considerations were applied to the insulin inputs to remove outliers or to be able to capture as much information as possible:
-
When the electric current infusion rate is not recorded, this is interpreted to mean that the rate has not inverse since the concluding information input, which is recorded in the ORIGINALRATE cavalcade (criterion I in Fig. i).
-
For regular insulin boluses, values < 18.0 U represent 99% of all values. For infusions, rates < 29.8 U/hour represent 99% of all entries. Values above the 99th percentile were adamant by clinical experts to be erroneous and excluded (criterion J for boluses and criterion I for infusions in Fig. 1). In all cases, values ≤ 0 were excluded (criteria I, J, and K in Fig. 1).
Once all these criteria were considered, the insulin data were incorporated with the curated subset containing the glucose readings (Fig. 1). Afterward, each regular insulin input, whether administered as a bolus or a alter in the rate of an infusion, was aligned to a glucose reading every bit explained below.
After merging the curated information, the longest length of stay (LOS) was most 102 days and the shortest less than i day. The latter accounts for 0.one% of the included ICU stays (12,210 ICU stays in full). On average, these patients take a LOS of 12.0 ± 13.0 days and a median of seven days. Withal, 1 day is the most frequent length of stay, which represents 10.7% of included ICU stays. Shorter stays or equal to i week gather over fifty.0% of included ICU admissions.
Glucose readings and insulin inputs time alignment
Associating the glucose readings with insulin inputs was the next stride. This task aimed to align each regular insulin upshot with a glucose measurement. From hither on, nosotros shall just focus on the regular insulin bolus administrations since these are the most common insulin input in MIMIC-Iii (Table 2). According to standardized ICU protocols, regular insulin administration should exist preceded by a blood glucose measurement.
The goal was to link each insulin dose with the nearest glucose measurement. For this circuitous task, the following rules were implemented:
-
Rule one: A glucose reading should precede a regular insulin assistants past up to 90 minutes. This basis for this time window was derived from the diabetic ketoacidosis guidelines which recommend measuring glucose values every 60 minutes while receiving an insulin infusion10. An boosted 30 minutes were added, ninety minutes in full, to this interval to account for the fourth dimension it may accept for providers to register the result. These fourth dimension intervals are within the recommendations11.
-
Rule 2: When a regular insulin effect was not preceded, but instead followed, by a blood glucose measurement, this glucose reading was paired with the regular insulin administration if they were recorded within xc minutes of each other.
-
Rule 3: Sometimes a regular insulin infusion/bolus appeared between ii blood glucose measurements. In this case, the college glucose value was paired with the regular insulin entry equally long every bit they were entered within 90 minutes of each other.
-
Rule 4: When a regular insulin bolus occurred very close to a regular insulin infusion charge per unit, it was assumed that the patient was given a bolus and then commenced on an infusion. Both regular insulin entries were paired with the preceding blood glucose measurement, or the posterior glucose reading in example its value was higher than the preceding claret glucose and was entered within xc minutes of the insulin dose.
-
Dominion 5: No glucose values below 90 mg/dL were paired with a subsequent regular insulin bolus or infusion. No clinician will treat this depression of a blood glucose value with a regular insulin bolus or infusion.
Based on time-postage stamp data and proposed rules described in methods, 110,011 out of 145,678 (75.5%) insulin events were paired with a corresponding glucose measurement. The assumptions gathered in rule i paired 86,913 insulin events to a preceding glucose reading, which is 79% of the total alignments (n = 110,011, Table 3). Information technology is followed by the second rule (8,841 occurrences), fourth rule (8,683 occurrences), and third rule (5,574 occurrences). The occurrences for the fifth dominion were not counted existence that this rule has an exclusion purpose instead of including a pair of glucose-insulin.
In Table 3 the per centum of not paired refers to the number of inputs registered at the ICU that were not aligned. The total inputs column includes data before admission, during a stay, and after discharge from the ICU. Sixteen insulin inputs (0.01% of curated insulin inputs) were excluded due to timestamps indicating that the insulin was administered outside the time recorded for ICU length of stay (criterion L in Fig. i).
Assays for technical validation
Several assays and analyses were done to provide testify for decisions fabricated during our information curation process. This farther increases the validity and transparency of the rules proposed in this work.
Symmetry
Excess kurtosis and skewness were estimated to characterize the empirical distribution of glucose readings by testing method. Skewness was estimated using the Fisher-Pearson coefficient as detailed in the documentation of the SciPy library in Python12.
Cess of fingerstick and lab analyzer understanding
Assessment of the understanding between fingerstick and lab analyzed glucose measurements was done by identifying the first fingerstick glucose test during the ICU stay and pairing information technology with the lab analyzed test closest temporally to this fingerstick test. These pairs were stratified by the duration of time betwixt the two measurements and resulted in 11,904 pairs of fingerstick – lab analyzer readings. A series of Banal-Altman plotsxiii were used to appraise the understanding betwixt the two testing types as a role of the time between the tests (Fig. 2). The graphs are further complemented with a locally weighted scatter plot smooth (LOWESS) for Δ glucose equally the mean of the paired fingerstick-lab analyzed values increases.
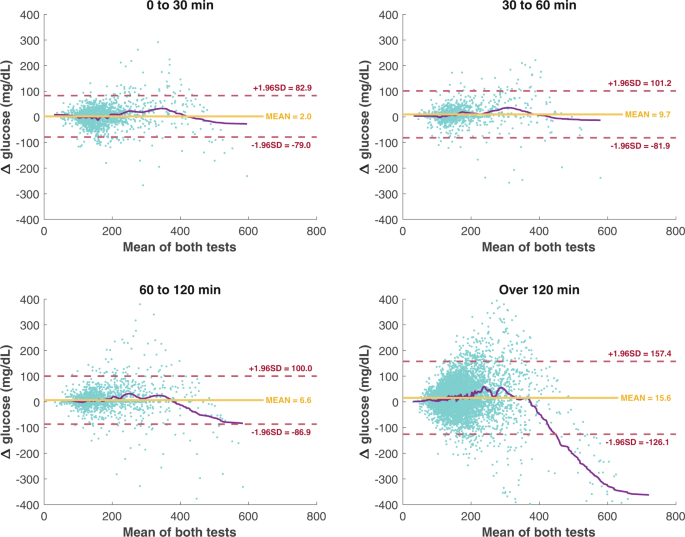
Agreement between both glucose readings methodologies. Bland-Altman plots of agreement between both glucose readings methods at 4 different time-gaps (∆ θ) or the time divergence betwixt a fingerstick reading and a sample analyzed in the chemistry lab (due north = eleven,904 paired readings). Each graph plots the mean value between a fingerstick reading and a lab analyzer sample (x axis), and Δ glucose (y axis). Horizontal lines delimit the mean difference or estimated bias (xanthous continuous line) and the upper and lower agreement limits (blood-red dashed lines) that highlight standard difference (SD) of Δ glucose. The purple continuous line plots the smoothed values (LOWESS) of Δ glucose.
Sample drove: comparison between pairing criteria
Independent samples were gathered to analyze and compare the unlike insulin-glucose pairing criteria discussed in this work. A pair composed of the get-go bolus of brusk-interim insulin and the corresponding preceding glucose reading were obtained per ICU stay for the three different cohorts aforementioned: (a) when a preceding glucose reading was recorded inside xc minutes of an insulin result, (b) when a preceding glucose reading was recorded within sixty minutes of the insulin effect, and (c) when no pairing rules were applied.
The departure between glucose readings in scenarios A and C; and between B and C were estimated (Δ glucose [mg/dL]). These estimated values were analyzed for hypothesis testing. They were further grouped depending on the temporal difference between an insulin issue and previous glycemic check (Δθ [minutes]): [0 30), [30 60), [sixty 90), [xc 120), [120 21,176).
We compared the glycemic check before the start insulin-effect every bit a function of these temporal differences. A paired Wilcoxon rank exam was used to appraise the nada hypothesis that the median departure in glucose measurements (scenario C vs A or B) was zippo. Statistical significance was assessed at the 0.05 level, and all tests were ii-sided.
Regression analysis
Lastly, we assessed if the frequency of fingerstick vs laboratory tests was associated with whatsoever admission, demographic, or clinical patient features. A multivariable logistic regression model was fit to identify covariates with an ICU admission having a higher number of bedside fingerstick readings over samples analyzed in the laboratory. Covariates were patient's age at admission, ICU admission type, ethnicity, gender, SOFA score, and diabetes status.
In the instance of the chiselled covariates of ethnicity and admission type, some categories were merged to form a more populated category. The admission types EMERGENCY (northward = nine,504) and URGENT (n = 143) were merged into an EMERGENCY category and compared to elective admissions. For ethnicity, the categories WHITE - BRAZILIAN, WHITE - EASTERN EUROPEAN, WHITE - OTHER EUROPEAN, and WHITE – RUSSIAN were grouped in the WHITE category and compared to all other ethnicities.
For elderly patients >90 years old (northward = 406), the age of these patients was imputed to 91.iv years (the median historic period among this group of patients, every bit historic period is otherwise withheld in MIMIC-III for regression analysis (https://mimic.physionet.org/mimictables/patients/). Regression analysis was performed on MATLAB version R2019b (The MathWorks, Inc.).
Data Records
When the curated glucose values were separated past method of measurement, 47.vi% were measured with laboratory equipment and 52.iv% were measured with the bedside glucometer (Tabular array 4). The mean value of glucose for the laboratory analyzer was 143.viii with a standard difference of ±64.2 mg/dL. The mean value of glucose for the fingerstick glucometer was 151.three with a standard deviation of ±59.3 mg/dL. Further, excess kurtosis and skewness values indicate that these readings do not have a normal distribution. Large kurtosis values signal that these still have large tail sizes, this value is larger in the samples for the laboratory analyzer. This is also confirmed with positive skewness (skewed correct), which is also detailed in Table 4.
The instances of insulin administration were curated to exclude insulin administered outside of the ICU and values which were zero or clinically impossible. This resulted in 145,694 instances of insulin assistants inside a population of 9,518 patients. The bulk of curation was performed on short-acting insulin. 3.v% of regular insulin values were excluded and 5.vii% of Humalog insulin was excluded. These results are summarized in Table 2. Notably, after the glucose values and insulin administration values were curated separately the population of patients in each group was exactly equal to 9,518.
Table five further shows the distribution of insulin based on the method of administration before and after curation. Both the raw and curated data have a bulk of insulin administrations given as short-acting insulin (91.1–90.8%) and of the short-acting type, almost are administered in boluses (69.8% vs. 69.4%).
Structure
A copy of each information subset has been uploaded to PhysioNet14 (read Usage Notes). The created subsets are 2 *.csv files named glucose_insulin_ICU and glucose_insulin_pair. Alternatively, these data subsets tin be created and downloaded into other file extensions (e.g.: JSON, etc.) with the assistance of the notebooks deposited on the associated PhysioNet projectxv (read Usage notes and Code availability).
The data subsets consist of time serial files that includes all the curated entries of glucose readings and insulin inputs. The file glucose_insulin_ICU.csv gathers the non-paired entries (16 columns); while the file glucose_insulin_pair.csv (21 columns) gathers the paired entries under scenario A (read Methods).
Description of fields
Mutual in both glucose_insulin_ICU.csv and glucose_insulin_pair.csv fifteen
SUBJECT_ID
It is a unique identifier for an individual patient.
HADM_ID
Represents a single patient's admission to the hospital.
ICUSTAY_ID
Unique identifier for a unmarried patient's access to the ICU.
LOS_ICU_days
Length of stay in days.
first_ICU_stay
True if information technology is the first admission to the ICU for a unmarried hospital admission.
TIMER
Gathers the timestamps for either the STARTTIME for a unmarried insulin input or the GLCTIMER for a unmarried glucose reading. It is used to order chronologically the events during a hospital access.
STARTTIME
A timestamp that depicts when the administration of an insulin event started.
INPUT
Dose for a single bolus of insulin in U.
INPUT_HRS
Insulin infusion rate in U/hr.
ENDTIME
A timestamp that specifies when an insulin input stops or an infusion rate was changed.
INSULINTYPE
Acting blazon of insulin: short, intermediate, or long (Table 2).
Effect
Specifies whether the bolus of insulin was subcutaneous (BOLUS_INYECTION), or intravenous (BOLUS_PUSH), or if the insulin was infused (INFUSION).
INFXSTOP
Indicates when an infusion of insulin was stopped.
GLCTIMER
A timestamp that depicts when a glycemic check was done.
GLC
Glycemia value in mg/dL.
GLCSOURCE
Reading method for a glycemic bank check: fingerstick (FINGERSTICK) or lab analyzer (BLOOD).
Specific to glucose_insulin_pair.csv 15
GLC_AL
Glycemia value in mg/dL for a paired glucose reading with a unmarried insulin input. This value should lucifer with the value in GLC of a preceding glucose reading according to the dominion practical for this pairing example.
GLCTIMER_AL
A timestamp that depicts when a glycemic check was done for a paired glucose reading. This value should lucifer with the timestamp in GLCTIMER of a preceding glucose reading according to the rule applied for this pairing case.
GLCSOURCE_AL
Reading method for a glycemic check that was paired with an insulin input. This value should lucifer with the GLCSOURCE value of a preceding glucose reading according to the rule applied for this pairing example.
RULE
The dominion practical for pairing a single insulin input with a preceding glucose reading.
Repeated
Indicates whether the associated glucose reading in this entry was paired with a subsequent insulin input charted in this table. These entries aid to place and verify which glucose readings were paired. The users have the option to remove this entry if it is user-friendly for amend readability.
Technical Validation
Glucose readings
We assessed the agreement of measurements made by bedside fingerstick tests versus those made in the laboratory. Pairing the first readings of both methods was not ever possible (n = 216) because during that ICU stay merely i reading is recorded or only i method was used to assess glycemia. In the 11,904 paired readings, the predominant gender for this analysis is male (n = half dozen,922 pairs) and females represent nearly 42% (northward = 4,982 pairs). Farther, in 10,488 ICU stays the patient survived and the remaining ane,416 died in the ICU. The lengths of ICU stay are between 129.8 minutes and 104.2 days with a mean of 296.iii ± 316.three hours. SOFA scores are between 0 and 21 units with a mean of four.7 ± three.three. Likewise, age is still within the Q1 and Q3 of the entire datasetthree.
The graphs in Fig. two is shown the Bland-Altman plots in four different time-gaps. Values of Δ Glucose <−400 mg/dL were not included to facilitate the comparing of all plots. They prove that the bias for tests temporally close together is relatively small. For instance, bias is nearly two points on average when the tests are conducted within thirty minutes. As seen in Fig. two, when the tests were measured in close temporal proximity, particularly when the average glucose is <200 mg/dL, the boilerplate difference betwixt fingerstick and laboratory-derived measurements is quite small-scale.
Wilcoxon rank test in each time-gap for ∆ glucose demonstrated that there is a difference betwixt both methods at 5% of significance. The results for each time-gap (time ranges expressed in minutes) are [0, xxx) median ∆ glucose = ii.0 mg/dL, Q1 – Qiii [−17.0, 21.0], P = 0.024; [30, 60) median ∆ glucose = iv.0 mg/dL, Q1 – Q3 [−4.0, 26.0], P < 0.001; [60, 120) median ∆ glucose = 0.0 mg/dL, Q1 – Q3 [−2.0, 18.0], P < 0.001; [120, 26,748] median ∆ glucose = 15.0 mg/dL, Q1 – Q3 [−thirteen.0, 44.5], P < 0.001. Although statistically meaning, the median difference between tests, particularly over the shortest fourth dimension periods are unlikely to be clinically meaning for the vast majority of patients.
In Tabular array 6, we study the factors associated with having more than fingerstick tests than laboratory results over an ICU-stay. In a multivariable logistic regression analysis, we found that older age, male gender, and beingness diabetic were independently associated with a statistically meaning college frequency of fingerstick tests. Furthermore, emergency admissions and in-hospital mortality were associated with more laboratory tests, also statistically significant. No statistically pregnant associations between ethnicity or severity of illness (SOFA) were found at the 0.05 level.
Pairing of glucose readings and insulin inputs
The frequency of each rule during the procedure of alignment (how many times these rules were applied) was determined and presented in the Methods section. The rates of pairing are presented in Tabular array 3. The highest charge per unit of pairing was seen with boluses of curt-acting insulin (eighty.five%). The highest rate of misalignment was noted with injections of intermediate-acting insulin (75.7%), followed past long-acting insulin (66.0%). The rules likely failed to capture an associated glucose value because medium and long-acting insulin administrations may be guided by estimates of basal glucose control such equally morning time pre-breakfast glucose or patient weight, rather than dictated past a glucose reading at the time of insulin assistants16.
Table 7 further describes the results of the pairing when stratifying past type of insulin. Boluses of short-acting were associated with the highest mean (187.seven mg/dL) and median (173.0 mg/dL) glucose values compared to infusions of curt-interim insulin. The latter were associated with the lowest mean (166.nine mg/dL) and median (145.0 mg/dL) glucose values. Long-acting insulin had the largest range of insulin values (180 Units) as referred to in Table vii.
The insulin-glucose alignments were displayed graphically to clinically validate the results. Figure 3a plots the density of each insulin infusion effect aligned with a preceding glucose reading. As serum glucose values rise, there is a tendency toward increasing doses for infusions of insulin. The almost frequent dose charge per unit was two.0–4.0 Units per 60 minutes to treat glucose values within a range of 115.0–140.0 mg/dL (i,952 events).
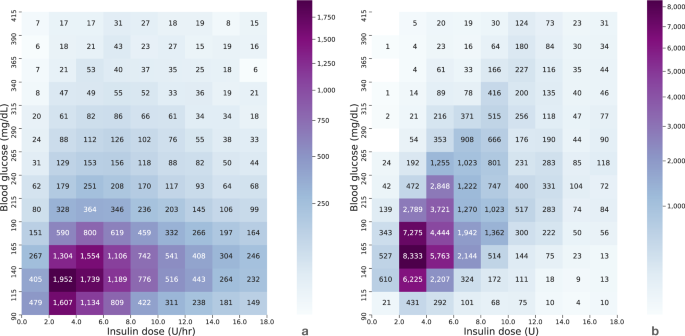
Preceding glucose readings paired with an insulin input. (a) Previous glucose readings of patients admitted to the ICU when an infusion of short-acting insulin administered (IV) starts, or changes infusion rate, or stops (n = 28,891). (b) Previous glucose readings when short-acting insulin boluses were administered (n =70,951). Glucose readings ≥415 mg/dL were not included in both plots to compare. Each cell represents the number of insulin - glucose pairs that fall within the specified range indicated along each axis.
Figure 3b plots the density of each glucose-insulin alignment for brusk-acting boluses. This density plot too follows the general practise of treating higher glucose values with higher insulin doses. The notable highlight of this figure is that the most frequently administered dose of short-interim insulin was 2–4 Units to treat glucose values in the range of 140–165 mg/dL (eight,333 occurrences). Comparing plots in Fig. 3, at that place is noticed that a higher density of doses for infusions were located in lower glucose readings compared to when boluses of curt-acting insulin were administered.
To complement this analysis, and to show the departure betwixt implementing and not implementing the proposed rules, ii additional cohorts were created to compare with the pairing criteria proposed above. The results of these comparisons are described in Table 8. Table 8 shows the glucose values paired to a bolus of insulin for a more liberal alignment window of 90 minutes every bit proposed previously (scenario A), a more conservative time window of threescore minutes (scenario B, additional cohort 1), and no fourth dimension window aligning (scenario C, additional accomplice 2). With fewer rules or constraints, a greater amount of data was gathered, in terms of the absolute number of entries. It is expected that an insulin event would pair with a glucose reading more frequently in the non-adjusted subset because it was subject to fewer constraints than the ii adjusted subsets. In other words, the not-adjusted subset (C) applies more simple criteria for pairing insulin events and glucose readings.
When no rules are considered, 89% alignment was achieved. Alignment percentage decreases as the maximum allowed time gap between an insulin issue and glycemic check decreases. The most notable difference amongst these subsets was in the range of glucose readings paired with an insulin administration. Specifically, glucose values below xc mg/dL (as depression as ii mg/dL) were paired with a bolus of regular insulin in the non-adjusted subset. This does not reflect what happens in the ICU. This pairing error can atomic number 82 to misleading conclusions if used to generate farther insights.
In Table nine, the statistical assay and comparison of scenarios A vs C and B vs C are presented. For both comparisons in all the periods, the zilch hypothesis was rejected. This demonstrated that the samples paired using the proposed rules were different than those paired when the rules were non applied. Moreover, the median difference between scenarios and percentiles (Qane and Q3) might exist clinically relevant for the vast majority of patients, especially over the largest fourth dimension-gaps.
In the concluding time-gap, there were 13 instances in our analysis where the recorded value of the outset glucose reading was the aforementioned in all scenarios. However, the recording time was completely dissimilar compared to scenario C. This demonstrates that the curation process should be carried out with well ascertain curation rules to gather accurate information for our analysis. Without careful and thoughtful curation of a dataset, subsequent analysis will inevitably provide misleading or flawed models.
The primary departure between scenario B and C was in the amount of information that was gathered to use for future analysis. Analysts should evaluate what is the best time-gap for the study they want to perform and how much information they want to keep. The more than information available, the more knowledge is bachelor to feed into a model or statistical assay. Thus, researchers should decide which timeframes adapt the best to the aim of their studies.
This manual team-based approach provides singled-out advantages to automated methods normally used in information scientific discipline to discover outliers and erroneous values (e.thousand.: statistical approaches based on parametric and non-parametric methods). The primary advantage of automated methods is that they are less fourth dimension consuming than the one proposed in this work. However, they may lead to inaccurate, or worse, biased models if flawed assumptions were encrypted during the data preparation. The team of data scientists and domain experts tin can iteratively interrogate the information and create rules to maximize fidelity to the clinical context. In addition, careful curation of the data must take into consideration various types of errors that are associated with data entry by clinical staff, which requires familiarity with the workflow. For instance, when a drug is administered, the data entry timestamp (shop fourth dimension) might be preceding the administration timestamp (chart time); or transmission entry of different labels of the aforementioned drug that creates several items ids associated with the drug. Thus, this procedure requires the careful creation of rules for processing information that balances the loss of the least amount of data with the removal of inaccurate data.
Usage Notes
The information that support the findings of this paper employs the MIMIC-Three data, a publicly available dataset3 that has been widely used in the analysis of existent-world health information17. The admission to these services is managed directly by PhysioNetxiv and researchers should request admission by themselves. They must sign a data use agreement, which outlines the information usage and security standards and prohibits any effort to identify the patients in MIMIC. This database is available as a collection of comma separated value (CSV) files. Further instructions to import them into dissimilar database systems are available on the MIMIC website (https://mimic.physionet.org/gettingstarted/dbsetup/).
The data subset copies are bachelor in PhysioNet14 under the projection name "Curated information for describing the claret glucose management in the intensive care unit of measurement"15. As an alternative, the 1_0_ara_curation_I.ipynb notebook details how to build the information subsets from the MIMIC-III tables. The 2_0_ara_pairing_II.ipynb notebook contains a hand-on case that shows how both glucose readings and insulin boluses tin can be paired with the rules proposed in this work.
The queries within the notebooks are optimized to be used on Google'due south BigQuery (SQL standard). The two JUPYTER notebooks can be run on Google's Colaboratory. In case the user runs these notebooks locally, the user should take installed JUPYTER notebooks and required dependencies and modules. The Alive Script requires at least MATLAB version R2019b. Alternatively, HTML copies of these Live Scripts are shared in the folder Notebooks (see Code availability).
The assumptions and rules, and their implementation, are provided in detail to serve as a starting bespeak for further refinement of the queries and subsequent analysis. While this study focused primarily on the management of hyperglycemia, the analysis of circumstances surrounding hypoglycemia is limited. Low glucose values were accounted for in the procedure of insulin pairing and tracking insulin infusion discontinuation. However, there remains an opportunity to analyze in more detail the management of hypoglycemia in the ICU. For example, tracking the glucose values that led to the decision to finish an insulin infusion would provide useful information to describe existent-world practice. The authors hope that this curated dataset will be used to further investigate trends in ICU glucose command and how relate to patient outcomes.
Code availability
All code used for information extraction, processing, and visualization is available online (two JUPYTER notebooks in Python three.7) and two MATLAB's Alive Script files) in the PhysionNet projection associated with the present paper15. These scripts are publicly bachelor to allow for reproducibility and lawmaking reuse. The associated PhysioNet project contains three folders. The Information binder contains the data subsets described in this paper. The content of the other folders is explained beneath.
Queries folder
Contains the queries to obtain the raw insulin entries and blood glucose readings. The queries tin be run on Google'due south BigQuery. The file glucose_readings.sql contains the code to excerpt glucose readings, and the file insulin.sql the codes for insulin entries.
Notebooks
Contains the following files:
JUPYTER notebooks
1.0-ara-information-curation-I.ipynb: This notebook contains the processing stages to obtain the curated entries of glucose readings and insulin inputs.
2.0-ara-pairing-II.ipynb: This notebook contains the pairing rules to link a preceding glucose reading with a regular insulin input.
MATLAB Live Scripts
Glucose_Analysis.mlx: This contains a deeper statistics assay on the glucose readings. Information technology is a complementary analysis for 1.0-ara-information-curation-I.ipynb notebook.
Pairing.mlx: Contains the results related to the pairing of a preceding glucose reading and an insulin event. Information technology is a complementary analysis for the ii.0-ara-pairing-II.ipynb notebook.
Glucose_Analysis.html & Pairing.html: Contain the same information every bit the scripts mentioned to a higher place, only readable in a spider web browser.
Functions subfolder:
Contains MATLAB functions that are called in the Live Scripts described above.
References
-
Malmberg, K., Norhammar, A., Wedel, H. & Rydén, L. Glycometabolic state at admission: important run a risk marker of mortality in conventionally treated patients with diabetes mellitus and acute myocardial infarction. Circulation 99, 2626–2632 (1999).
-
Baker, L. et al. Real-world characterization of blood glucose control and insulin use in the intensive intendance unit of measurement. Sci. Rep. 10, 10718 (2020).
-
Johnson, A. Eastward. Due west. et al. MIMIC-III, a freely attainable critical care database. Sci. Information iii (2016).
-
MIT Disquisitional Data. Secondary Analysis Of Electronic Health Records. (Springer International Publishing, 2016).
-
Wu, J., Roy, J. & Stewart, West. F. Prediction modeling using ehr data: challenges, strategies, and a comparison of auto learning approaches. Med. Care 48, S106–S113 (2010).
-
Clifford, M. D., Long, West. J., Moody, Thousand. B. & Szolovits, P. Robust parameter extraction for decision support using multimodal intensive care data. Philos. Trans. A. Math. Phys. Eng. Sci. 367, 411–29 (2009).
-
Corrigan-Curay, J., Sacks, L. & Woodcock, J. Existent-world testify and real-world data for evaluating drug safety and effectiveness. JAMA 320, 867 (2018).
-
Sherman, R. E. et al. Real-world evidence — what is it and what can information technology tell us? N. Engl. J. Med. 375, 2293–2297 (2016).
-
Laposata, M. In Laposata's Laboratory Medicine The Diagnosis Of Disease In The Clinical Laboratory 3rd edn Ch. two (McGraw-Hill Education LLC, 2019).
-
Kitabchi, A. E., Umpierrez, Grand. E., Miles, J. M. & Fisher, J. N. Hyperglycemic crises in adult patients with diabetes. Diabetes Care 32, 1335–1343 (2009).
-
American Diabetes Clan. xv - Diabetes care in the hospital: standards of medical care in diabetes. Diabetes Intendance 43, S193–S202 (2020).
-
Virtanen, P. et al. Scipy 1.0: primal algorithms for scientific computing in python. Nat. Methods 17, 261–272 (2020).
-
Altman, D. 1000. & Bland, J. Chiliad. Measurement in medicine: the assay of method comparison studies. Stat. 32, 307 (1983).
-
Goldberger, A. L. et al. Physiobank, physiotoolkit, and physionet: components of a new research resource for complex physiologic signals. Circulation 101, E215–20 (2000).
-
Robles Arévalo, A., Mateo-Collado, R., & Celi, L. A. Curated data for describing the claret glucose management in the intensive care unit. PhysioNet https://doi.org/x.13026/d18t-tf45 (2021).
-
American Diabetes Association. viii - Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes. Diabetes Care 41, S73–S85 (2018).
-
Johnson, A. East. West., Rock, D. J., Celi, L. A. & Pollard, T. J. The mimic code repository: enabling reproducibility in disquisitional care research. J. Am. Med. Information science Assoc. 25, 32–39 (2018).
Acknowledgements
The piece of work of A.R.A. was supported past the PhD fellowship PD/BD/114107/2015 from Fundação da Ciência eastward da Tecnologia (FCT). The work of A.R.A., S.Thousand.S.V., and J.Thousand.C.S. was supported through IDMEC, under LAETA, projection UIDB/50022/2020; as well, by the European Regional Development Fund (LISBOA-01-0145-FEDER-031474) and FCT through Programa Operacional Regional de Lisboa (PTDC/EME-Sis/31474/2017). The Medical Information Mart for Intensive Care is funded by the National Institute of Health through the NIBIB grant R01 EB017205. The data in MIMIC-III has been de-identified, and the institutional review boards of the Massachusetts Establish of Technology (No. 0403000206) and Beth Israel Deaconess Medical Center (2001-P-001699/14) both approved the use of the database for research. The authors would similar to thank to the Laboratory for Computational Physiology (LCP) at MIT for helpful feedback regarding the deposition of our codes in PhysioNet and reproducibility of our report.
Author information
Affiliations
Contributions
All authors contributed to writing the manuscript. A.R.A., Fifty.B. and J.Chiliad. collaborated on the information extraction, visualization, and analysis. J.M., J.D.R., R.Grand., Fifty.A.C. and F.D. interpreted, validated results, blueprint of the work and supervised data extraction. J.M.C.S., S.Thou.S.V. and S.F. reviewed the paper and supervised the piece of work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, accommodation, distribution and reproduction in whatsoever medium or format, as long every bit you give appropriate credit to the original author(s) and the source, provide a link to the Artistic Commons license, and point if changes were made. The images or other 3rd party material in this article are included in the article's Artistic Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons license and your intended employ is non permitted by statutory regulation or exceeds the permitted employ, you will need to obtain permission direct from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/iv.0/.
The Artistic Commons Public Domain Dedication waiver http://creativecommons.org/publicdomain/zero/1.0/ applies to the metadata files associated with this article.
Reprints and Permissions
Most this commodity
Cite this article
Robles Arévalo, A., Maley, J.H., Baker, L. et al. Information-driven curation procedure for describing the blood glucose management in the intensive care unit. Sci Data 8, 80 (2021). https://doi.org/10.1038/s41597-021-00864-4
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1038/s41597-021-00864-four
Source: https://www.nature.com/articles/s41597-021-00864-4?error=cookies_not_supported&code=ee3a4b16-607e-4c32-a8a4-86efb5e689b9
0 Response to "Is Glucose Reading of 89 in Morning Good?"
Post a Comment